GroupNews – September 2021
Eckler’s GroupNews monthly newsletter provides commentary on the issues affecting Canadian group benefit plans.
In this edition:
- Ontario optometrists withdraw from OHIP
- Manitoba expands coverage for diabetes
- Trend projections for 2022 for health and dental plans
- Federal government releases regulations to limit therapeutic product shortages
- Ontario introduces process for WSIB to recover overpayments made to employers with respect to Infectious Diseases Emergency Leave
- Employment Insurance premium rate announcement for 2022
- Impact of COVID-19 on Canadian healthcare systems remains uncertain
Benefit plan management
Ontario optometrists withdraw from OHIP
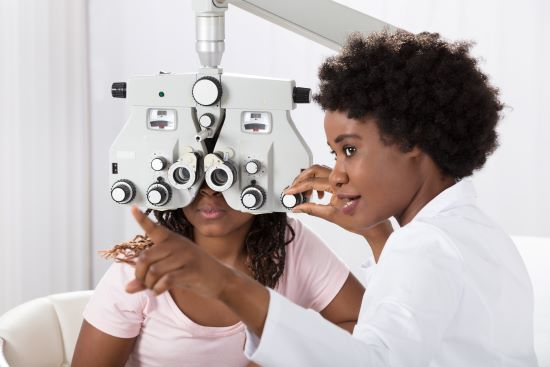 The Ontario Association of Optometrists has announced its withdrawal from Ontario’s Health Insurance Plan (OHIP) on September 1, 2021. The optometrist’s association made the decision to withdraw from OHIP due to the lack of funding received from OHIP for the cost of eye exams.
The Ontario Association of Optometrists has announced its withdrawal from Ontario’s Health Insurance Plan (OHIP) on September 1, 2021. The optometrist’s association made the decision to withdraw from OHIP due to the lack of funding received from OHIP for the cost of eye exams.
Prior to the withdrawal, OHIP paid for one annual major eye exam (vision and general eye health) for Ontario residents aged 19 or younger and 65 and over, and for other residents with specific medical conditions. Current Ontario regulations prohibit optometrists from billing directly to patients, workplace health insurance or to individual private insurance for any services provided to those eligible under OHIP.
Due to the withdrawal from OHIP, optometrists may refuse to provide routine eye exams to Ontario residents eligible for OHIP coverage. The refusal may result in missed opportunities for early detection of eye diseases for patients under the age of 19 or over the age of 65.
Impact: The withdrawal from OHIP will not result in increased claims for these age cohorts as optometrists were already prohibited from billing workplace health insurance or private insurance for services, nor does it affect eligible plan members aged 20 to 64 as services were not covered by OHIP prior to the withdrawal of services. It may, however, cause delays in services for eligible residents unless an agreement is reached between the province and the association.
Benefit plan management
Manitoba expands coverage for diabetes
First announced in the 2021–22 provincial budget, the Manitoba government is moving forward with expanding coverage under the provincial insulin pump program.
 The program, which covers the cost of advanced glucose monitors and insulin pumps for people under the age of 18 with Type 1 diabetes, is expanding to include those under the age of 25. The government estimates the expanded program will provide more than 1,000 Manitobans coverage for advanced glucose monitors, and coverage for up to 200 Manitobans for insulin pumps. The new funding for advanced glucose monitors comes into effect on September 28, 2021, and in November 2021 for insulin pumps.
The program, which covers the cost of advanced glucose monitors and insulin pumps for people under the age of 18 with Type 1 diabetes, is expanding to include those under the age of 25. The government estimates the expanded program will provide more than 1,000 Manitobans coverage for advanced glucose monitors, and coverage for up to 200 Manitobans for insulin pumps. The new funding for advanced glucose monitors comes into effect on September 28, 2021, and in November 2021 for insulin pumps.
Impact: While individuals will not be required to meet their pharmacare deductible for insulin pumps, the deductible amount will be applied to the advanced glucose monitors. While expected to be relatively minor, employer plans with costs under the expanded age group should experience some savings as the pharmacare is first payor in the province. Coverage for advance glucose monitors will also help with improved self-management of diabetes, which could provide cost savings from the potential reduction of additional healthcare treatment.
Benefit plan management
Trend projections for 2022 for health and dental plans
 In Eckler’s March 2021 GroupNews publication, we reported on trends shared with us by insurers as their outlook for 2021. The insurers surveyed cited (prospective) annual trend factors ranging from 11.2% to 13.0% for extended health inclusive of drugs, vision, paramedical and other services. When determining trend factors for dental, the insurers expected a 3% to 7% utilization trend plus a fee guide adjustment of up to 5%. These projections are based on the claiming patterns of insurers’ books of business that are comprised of various financial arrangements, which come into play in how they apply trends and the factors they use in their rate-setting process.
In Eckler’s March 2021 GroupNews publication, we reported on trends shared with us by insurers as their outlook for 2021. The insurers surveyed cited (prospective) annual trend factors ranging from 11.2% to 13.0% for extended health inclusive of drugs, vision, paramedical and other services. When determining trend factors for dental, the insurers expected a 3% to 7% utilization trend plus a fee guide adjustment of up to 5%. These projections are based on the claiming patterns of insurers’ books of business that are comprised of various financial arrangements, which come into play in how they apply trends and the factors they use in their rate-setting process.
Not surprisingly, our retrospective trends in 2020 vs. 2019 were not unlike others where we saw:
- an overall decrease of 5.3% for extended health (made up of +5.6% for drugs and -14.9% for other health services); and
- a decrease of 20.7% for dental.
Trend factors play a significant role in the prospective renewal rate-setting of health and dental benefits. Beyond annual increases in the cost of the goods and services offered under these benefits, trend factors represent anticipated changes in utilization by eligible plan members, as well as the impact of external forces on the cost of coverage. For example, COVID significantly impacted the availability and usage of services in the first half of 2020, directly resulting in lower per capita cost under benefit programs. Claim levels rebounded beginning in July 2020 and continued into 2021, returning to 2019 pre-COVID levels.
Larger plans will exhibit their own trends, which should be the primary driver of renewal pricing for those plans, and where a plan has less credible patterns, overall trend patterns are typically utilized.
Impact:
Reflecting on trends for Eckler’s block of business over the prior year (2020 vs. 2019) and emerging 2021 experience, consisting of both active and retired plan members and covering plan sponsors in both the public and private sectors, GroupNews makes the following early recommendations for 2022 for those plans whose actual trend is not fully credible:
– between 6%–8% for drugs, 6%–10% for other Health components; and
– 5%–7% for Dental (inclusive of a 3–5% assumption for fee guide increases).
Legal and legislative news
Federal government releases regulations to limit therapeutic product shortages
 The federal government has released Regulations Amending Certain Regulations Concerning Drugs and Medical Devices (Shortages) SOR/2021-199 (Regulations) to address therapeutic product shortages that affect Canadians.
The federal government has released Regulations Amending Certain Regulations Concerning Drugs and Medical Devices (Shortages) SOR/2021-199 (Regulations) to address therapeutic product shortages that affect Canadians.
In response to global supply issues brought on by COVID-19, particularly with respect to drug shortages, the Regulations introduce exceptions to existing importation regulations under the Food and Drug Regulations and Medical Devices Regulations. This will allow the government to permit the importation and sale of products that do not fully meet Canadian regulatory requirements, but that are manufactured to comparable quality standards, to address anticipated or existing shortages. The amendments also provide Health Canada with additional tools to assess existing or potential shortages of certain drugs or medical devices, including gathering information from manufacturers on discontinuances and prohibit drug establishment licence holders from selling certain drugs intended for the Canadian market outside of Canada if the sale could cause or exacerbate a shortage.
Health Canada notes that during the early stages of the pandemic, there were 592 drug shortages reported in Canada, compared to 441 during the same period in 2019. This included 47 Tier 3 drug shortages, versus 10 Tier 3 shortages in 2019. Health Canada defines a Tier 3 drug shortage as those that have the greatest potential impact on Canada’s drug supply and healthcare system. Impact is based on low availability of alternative supplies, ingredients or therapies.
Impact: The amendments are expected to improve Health Canada’s ability to monitor, prevent and alleviate shortages in therapeutic products and better support healthcare systems across the country as they continue to recover from COVID-19. Preventing shortages will reduce the time spent by healthcare professionals searching for substitutes for products experiencing a shortage and will prevent patients from deferring necessary treatments.
Legal and legislative news
Ontario introduces process for WSIB to recover overpayments made to employers with respect to Infectious Diseases Emergency Leave
 On April 29, 2021, the Ontario government enacted Bill 284, COVID-19 Putting Workers First Act, 2021 (Act). The Act provides for Infectious Disease Emergency Leave (IDEL) pay to allow certain employees up to three days of paid leave for COVID-19 related reasons. Employers who provide IDEL may apply to the Workplace Safety and Insurance Board (WSIB) to be reimbursed, up to a maximum of $200 per day, per employee. The temporary sick leave program is set to expire on December 31, 2021.
On April 29, 2021, the Ontario government enacted Bill 284, COVID-19 Putting Workers First Act, 2021 (Act). The Act provides for Infectious Disease Emergency Leave (IDEL) pay to allow certain employees up to three days of paid leave for COVID-19 related reasons. Employers who provide IDEL may apply to the Workplace Safety and Insurance Board (WSIB) to be reimbursed, up to a maximum of $200 per day, per employee. The temporary sick leave program is set to expire on December 31, 2021.
On September 3, 2021, the Ontario government filed O. Reg. 637/21 (Regulation) made under the Ontario Employment Standards Act, 2000. The Regulation sets out the process to recover an overpayment made by the WSIB for paid IDEL from an employer. Employers will be ordered to pay the overpayment amount as well as administrative costs equal to the greater of $100 and 10% of the overpayment.
Impact: As reimbursement for IDEL is not paid out of the WSIB insurance fund, we do not anticipate any impact on WSIB-related costs to employers.
Legal and legislative news
Employment Insurance premium rate announcement for 2022
Each year, the Canada Employment Insurance Commission sets the annual premium based on the
seven-year break-even rate as forecasted in the Actuarial Report on the Employment Insurance (EI) Premium Rate (Report). The break-even rate is forecasted by the EI Senior Actuary to be $1.81 per $100 of insurable earnings from 2022 to 2028, balancing the EI operation account at the end of 2028.
In 2020, the federal government announced that due to the economic impact of COVID-19, there would be a temporary freeze on the EI rates for 2021 and 2022. The rate will remain at $1.58 per $100 of insurable earnings for 2022.
EI premium rates for Quebec residents (who are covered under the Quebec Parental Insurance Plan) will be $1.20 per $100 of insurable earnings for employees and $1.68 per $100 of insurable earnings for employers, up from $1.18 and $1.65 respectively.
Maximum insurable earnings for 2022 will increase to $60,300 from $56,300 in 2021.
Impact: The break-even rate forecasted in last year’s report has decreased from $1.93 per $100 of insurable earnings and could be an indication that future premium increases may not be as large as indicated last year.
Research
Impact of COVID-19 on Canadian healthcare systems remains uncertain
 Recently released data from the Canadian Institute for Health Information (CIHI) examines how the pandemic has affected Canada’s healthcare system. The study on the Impact of COVID-19 on Canada’s healthcare systems explores emergency department visits, access to hospital care and how Canadians received care from physicians during the period from March, when the pandemic began, to December 2020 (and compares it to the same period in 2019.)
Recently released data from the Canadian Institute for Health Information (CIHI) examines how the pandemic has affected Canada’s healthcare system. The study on the Impact of COVID-19 on Canada’s healthcare systems explores emergency department visits, access to hospital care and how Canadians received care from physicians during the period from March, when the pandemic began, to December 2020 (and compares it to the same period in 2019.)
Emergency department visits
- Across Canada, visits to emergency departments declined by almost 25,000 a day by April 2020 when compared to April 2019. This is about half the usual volume Canada’s emergency departments would typically see. By the end of 2020, visits to emergency departments declined by approximately 13,300 a day.
- Although emergency department activity significantly declined during the first wave of the pandemic, people with unplanned health concerns did receive care. Less urgent and non-urgent visits decreased the most, by about 50%, followed by urgent and emergent visits, at just more than 40%. Overall, fewer people sought care for common health concerns such as colds and flu, as well as for more significant concerns like cardiac events and trauma.
Access to hospital care
- From March to June 2020, overall surgery numbers fell 47% compared with 2019, representing about 335,000 fewer surgeries. This is a reflection of the response from the health authorities across the country to cancel planned surgeries in preparation for a potential surge of COVID-19 patients. By the end of 2020, the number of surgeries rebounded, with December having only 4% fewer surgeries when compared to December 2019. Overall, there were 22% fewer surgeries from March to December 2020 when compared to the same period in 2019.
How Canadians received care from physicians
- The number of patient visits (both in person and virtual) to all physicians dropped by 13% during the early period of the pandemic, from March to June 2020. Not surprisingly, the percentage of virtual visits increased significantly in 2020 in all provinces where data is available.
Impact: Canadians’ comfort with seeking healthcare during the Covid-19 pandemic along with the public health messaging about social distancing and government policies to slow down surgeries in 2020 had a significant impact on the healthcare system. With the emergence of variants of concern and the continuing increase in case numbers, we do not yet have the full picture of the impact of delayed or deferred care.
This publication has been prepared by the GroupNews editorial board for general information and does not constitute professional advice. The information contained herein is based on currently available sources and analysis. The data used may be from third-party sources that Eckler has not independently verified, validated, or audited. They make no representations or warranties with respect to the accuracy of the information, nor whether it is suitable for the purposes to which it is put by users. The information is not intended to be taken as advice with respect to any individual situation and cannot be relied upon as such.
Current editorial board members are: Andrew Tsoi-A-Sue, Ellen Whelan, Charlene Milton, Philippe Laplante, and Nick Gubbay.